Complications After Cataract Surgery
 Cataract surgery is one of the most common surgeries in the United States today. It can be one of the safest and most successful surgeries a patient may experience in their lifetime. Yet like with any surgery, there is always a risk for complications. Some known risks of cataract surgery include infection, eye floaters, scar tissue formation, inflammation, lens dislocation, glare, halos, droopy eyelid, high eye pressure, retinal tear, or retinal detachment. Your ophthalmologist may refer you to a retina specialist for a consultation if specialized retina care is needed after cataract surgery.
Cataract surgery is one of the most common surgeries in the United States today. It can be one of the safest and most successful surgeries a patient may experience in their lifetime. Yet like with any surgery, there is always a risk for complications. Some known risks of cataract surgery include infection, eye floaters, scar tissue formation, inflammation, lens dislocation, glare, halos, droopy eyelid, high eye pressure, retinal tear, or retinal detachment. Your ophthalmologist may refer you to a retina specialist for a consultation if specialized retina care is needed after cataract surgery.
A common complication after cataract surgery is cystoid macular edema or CME. After cataract surgery there varying degrees of inflammation in the eye. This inflammation is usually controlled by using steroid eye drops for several weeks, included in a common drop regimen directed by your surgeon. In some cases, the macula can develop pockets of fluid within the retina causing swelling/edema. This edema usually causes a noticeable decrease in vision in the surgical eye. The vision after surgery can be initially quite good then degrade slowly over time as the edema develops. Depending on the severity of the swelling, your ophthalmologist may make changes to your post-operative drop regimen. Your surgeon may refer you to a Retina Specialist or Retinologist for further management and treatment. This swelling is more common if you are a diabetic or if your retina has been damaged in the past by a retinal detachment or vein occlusion.
The retinologist will dilate the pupils and perform a series of specialized tests to determine the severity of the CME. If the CME is not responding well to eye drops, the retinologist may administer a dose of steroidal medication by injecting it directly into the tissues around the eye or into the eye. These injections are not usually painful and deliver the steroids near the macula for a more potent dose. CME can take several weeks to months to completely clear up, in which time you will have periodic visits with the retina specialist. Once the CME has resolved, the retina specialist will return you to your cataract surgeon for an eyeglass prescription exam.
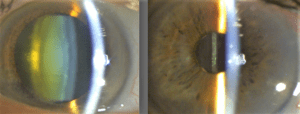
Another complication from cataract surgery can be a dislocated intraocular lens or IOL. When a cataract is removed it is replaced with a PC (Posterior Capsule) IOL. The PC IOL sits inside of a natural sack which is supported by many tiny threads called zonules. Sometimes during surgery, the zonules can become loose, weak, and even break. Weakened or broken zonules can cause the IOL to fall away from its central position behind the iris (the colored part of the eye) and dislocate. A sudden and significant decrease in vision is what patients notice. It can dislocate at the time of cataract surgery or at any time after it is implanted. When the IOL dislocates, it often needs to be removed and replaced.
This secondary cataract surgery operation is actually several procedures combined. The retinal surgeon will carefully perform a vitrectomy. A vitrectomy is a removal of the vitreous (jelly) that fills the space in the eye between the IOL and the retina. This removes the tension from the retina so the lens can be safely removed. The lens is usually removed through the prior cataract surgery incision. After this delicate procedure is performed, the cataract surgeon will place an AC (Anterior Chamber) IOL in front of the iris. There are other locations where a lens can be placed within the eye depending on the structural integrity of a patient’s eye anatomy. Within anywhere from the next day to a few weeks, retina specialists hope for a dramatic improvement in the vision.
